
BLOG
Our health stories
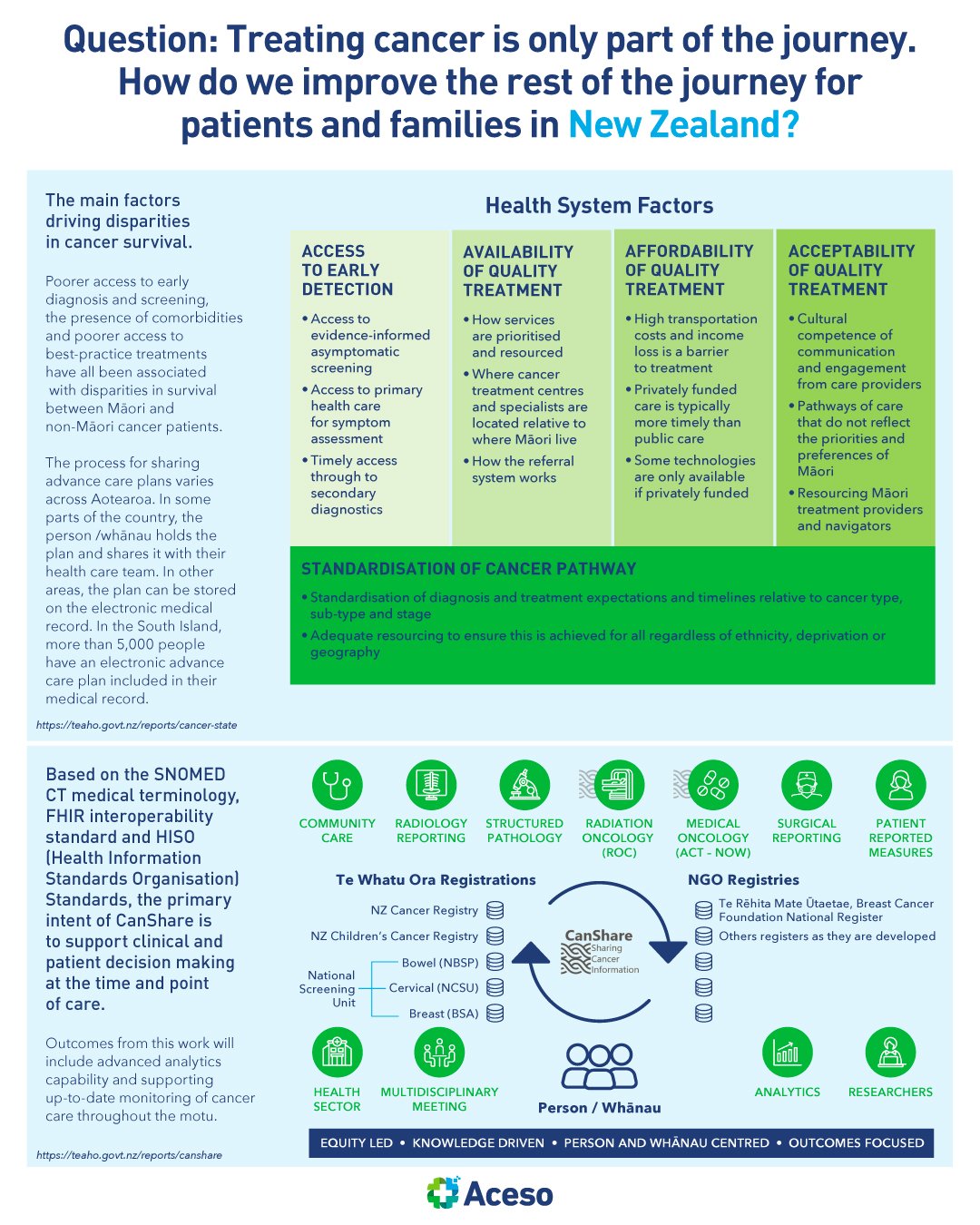
Treating cancer is only part of the journey. How do we improve the rest of the journey for patients and families in New Zealand?
We have many world class aspects of cancer control in New Zealand, and the cancer workforce is full of highly committed and talented people, but if we are to improve our cancer survival rates compared to similar countries, focused action is needed

How do we achieve equitable access to medicine in New Zealand?
By failing to invest, New Zealand misses out on the savings to the health system and economic benefits that modern medicines offer. With this in mind, how do we make improvements to safeguard the future of our healthcare sector?

Data and insights that help governments prioritise health challenges and allocate resources, rely on robust country-wide health information systems. How is New Zealand tracking?
Transparent, accurate and accessible information enables patients and the public to know whether the services they are receiving are high quality, efficient and effective. Equally, clear and effective engagement with the public builds confidence that individuals’ data contributions are creating real benefits for themselves and wider society, thus underpinning further improvement and transformation.

Women and health are key to sustainable development. In July 2023, New Zealand will share its first ever Woman’s Health Strategy. What can we expect from it?
While Aotearoa is a relatively progressive country regarding women's health, there are still barriers that women face in accessing healthcare and achieving optimal health outcomes. The countries that perform best in terms of women’s care outcomes have high levels of gender equality, access to healthcare, and other social and economic factors that contribute to women's well-being.

How can New Zealand attract the finite healthcare workforce resource?
Health systems can only function with health workers; improving health service coverage and realising the right to the enjoyment of the highest attainable standard of health is dependent on their availability, accessibility, acceptability and quality.

How do we create a fit-for-purpose regulatory framework for digital health in New Zealand?
The rapid uptake of such digital tools points to an area ripe with opportunity to improve and complement existing health care services and reach historically underserved populations. But to fully realise the benefits of novel digital offerings, concomitant innovation in regulatory pathways is necessary.

How do we improve healthcare rehabilitation pathways in New Zealand?
Are we are stuck dependent on an under-funded and inefficient system that could be preventing people from reaching their full potential unless they have the means to do it themselves?

What is the changing role of allied health professionals in New Zealand’s evolving healthcare landscape?
It might be worthwhile to begin with answering the transdisciplinary riddle: What is it that you do and you need to do and only you can do, as opposed to what is it that you do, that needs to get done, but you do not necessarily need to do?

How do we approach change management in New Zealand within the healthcare sector?
Change is indeed more work. Those closest to the change in terms of designing and testing it are often overloaded, in part because of the inevitable unanticipated glitches per “Kanter’s Law” that “everything can look like a failure in the middle.”
Healthcare companies first need to identify and prioritise their critical sources of value. Second, they must build their service-delivery capabilities. Third, they should look for ways to modernise their IT foundations. And fourth, companies must ensure that they build and maintain core management competencies.

Question: What can we do to reflect the role and worth of NPs in New Zealand?
The nurse practitioner (NP) role was launched in New Zealand in 2001, and described by the Ministry of Health as "a way of combining the best of nursing with some skills from medicine". Since then, NPs have been providing highly skilled care to patients , many choosing to work in primary and community care. More and more New Zealanders are now enrolled with an NP as their primary health care provider.

Question: Oral health in New Zealand has been lagging. How do we address the impending crisis?
Our health system is being transformed with the aim of providing health services that are more accessible and equitable for all people in Aotearoa New Zealand. As part of this transformation, the time has come for health care at the first point of contact, GPs and dentists, to be made free to all the people who need to use them.
Publicly funded hospitalisation rates for oral health increased by 31% from 2007/08 to 2018/19, while the population increased by 17% over the same period. Dental caries is the main reason for hospitalisation, amounting to 58% of all oral health hospitalisations in 2018/19. Hospitalisations for other conditions such as heart disease, which may be linked to unmet oral health need, are not included in these statistics. Most oral health conditions are largely preventable and can be treated in their early stages.

Question: Is it time to revisit prescription charges in New Zealand?
Forgoing medicines may also lead to more health costs in the future, as conditions go untreated and complications arise, leading to emergency care and hospital visits. Reducing the price of prescription medicines will mean more people will be able to afford them, with the health and other benefits it brings.

Children’s immunisation rates - how does New Zealand fare?
Over the past 2 years, while our attention was focused on Covid-19, with a huge effort to vaccinate against it, all those other diseases didn’t attract the same attention, leading to falling vaccination rates. Officials in NZ are particularly concerned with access to healthcare, especially the rising cost of transport and delays in accessing general practices. The COVID-19 vaccination experience has also shown how Māori and Pacific community health providers can help reach high vaccination targets, especially when combined with good outreach services, increasing vaccination providers beyond GP clinics, and building the vaccination workforce.
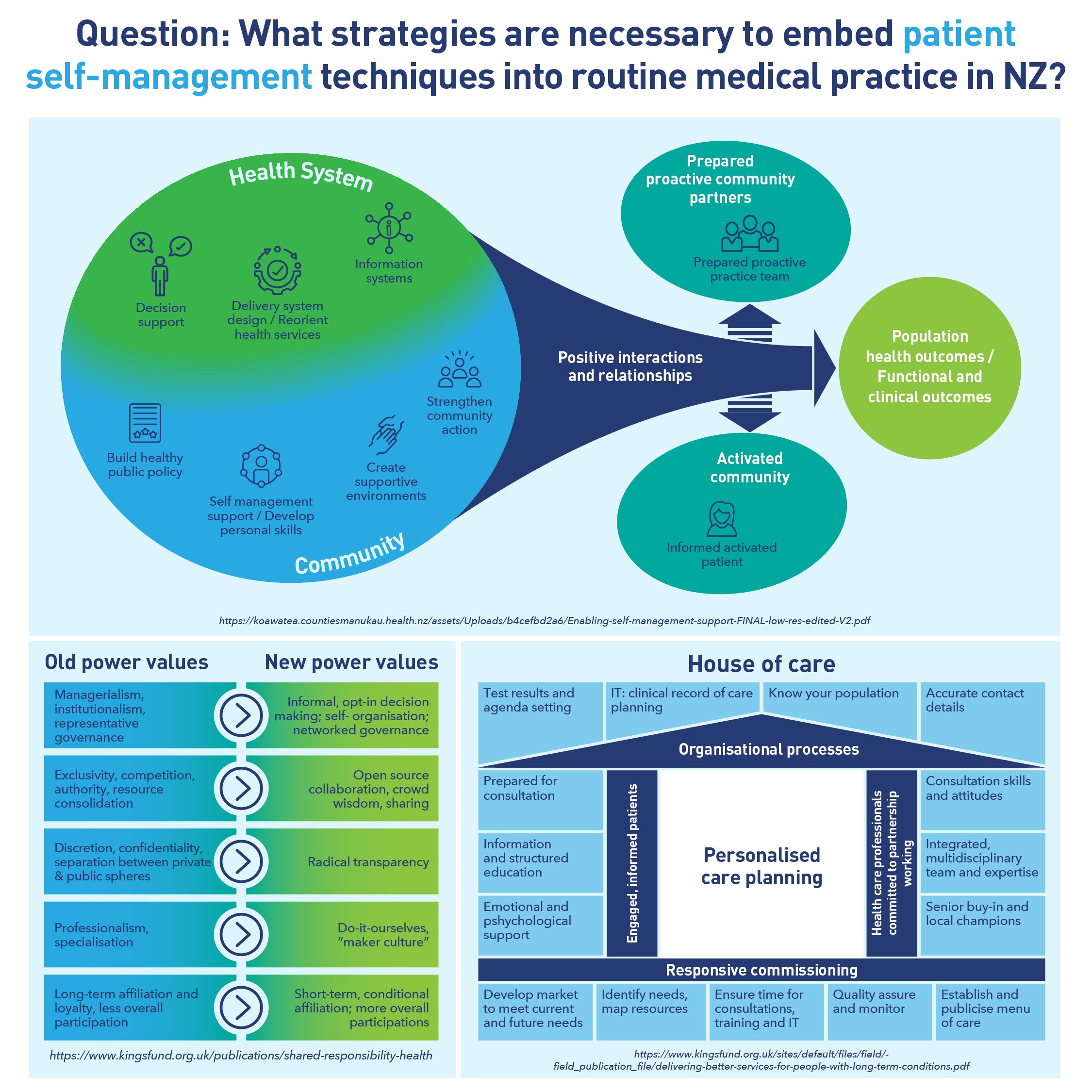
What strategies are necessary to embed patient self-management techniques into routine medical practice in NZ?
LTCs are rising in New Zealand and many people have several LTCs. These include diabetes, cancers, cardiovascular diseases, respiratory diseases, mental illness, chronic pain, chronic kidney disease, dementia and others. Supporting people to self-manage is a critical part of coping with the growing burden of LTCs.

What is the role of organisational culture in healthcare?
Fostering the right culture in healthcare organisations is essential to ensure they provide compassionate, high-quality care for patients. This requires the creation of transparent cultures in which mistakes are viewed as learning opportunities, where staff can raise concerns and know the appropriate action will be taken, and honesty and openness is promoted. The most important determinant of the development and maintenance of an organisation’s culture, including cultures of compassionate care, is leadership. Every interaction by every leader at every level shapes the emerging culture of an organisation.

Is digital health closing gaps in health equity in New Zealand?
Inequity in society is reflected in digital health equity, thus, those at risk of social exclusion (ie, those at a disadvantage due to, for example, unemployment, low education, and a weak economic situation) are also at greater risk of being excluded from digital health services . The rapid digitalisation of health services has posed a considerable risk of increasing digital inequality, which in turn may cause significant disadvantages such as an increased risk of health deterioration, exposure to COVID-19 if the necessary services cannot be obtained remotely, and social isolation, especially for those who already are in a vulnerable position. Concerns have been raised about whether particularly those, who may not have equal access, ability or resources to use digital services have received the health services they need.

Question: How do we address gaps in mental health services for youth and children in New Zealand?
There is evidence that in healthcare, the best return on investment for future wellbeing is made between the years of 0-4 years. While it may be difficult for the wider health system to commit to a long term view, investment in early childhood is likely to provide the greatest gains in improving overall mental health outcomes.

Question: Is health insurance a highly ‘sought after’ benefit among New Zealand employees?
Multiple large-scale surveys have found compelling evidence that employee attrition is at record levels. Health benefits can help employers attract and retain employees. According to a McKinsey report, compared with before the pandemic, the proportion of employers reporting that benefits are “very important” in talent management increased by 11%.

Does New Zealand’s healthcare system have a mature cybersecurity posture?
In the future of health, data will be more widely shared, collected, and analysed. Healthcare organisations will be positioned to create new value from this previously unavailable information, using it to drive operational efficiencies and help enhance consumer engagement. As this transformation advances, organisations will need to pay closer attention to data privacy and take steps to modernise data protection standards. They will also face added pressure to establish better cyber threat awareness, detection, and response capabilities. Ironically, the more digital that healthcare becomes, the more vulnerable it is to threat actors.

Are New Zealand’s pathology and laboratory services ready to respond proactively to future changes and challenges?
It is generally accepted that approximately 70% of diagnoses rely on output from pathology, diagnostic imaging or laboratory services. Significant change will occur in the New Zealand public health system over the next ten years which will impact on the pathology and laboratory service sector. There is a dire need for policy-makers, managers and practitioners to balance quality of care with the cost of services.
