
BLOG
Our health stories

Is population ageing a good measure of the success of our healthcare system?
A range of factors influence an individual’s use of health services, including: health status, the price of services, incomes, individual preferences, whether they are covered by health insurance and characteristics such as age, gender and ethnicity. Medical technology and pharmaceutical advances along with improved healthcare services help today’s older New Zealanders to be more confident, assertive and active than previous older generations. Preventative and primary healthcare are also important to help them enjoy good health for as long as possible.
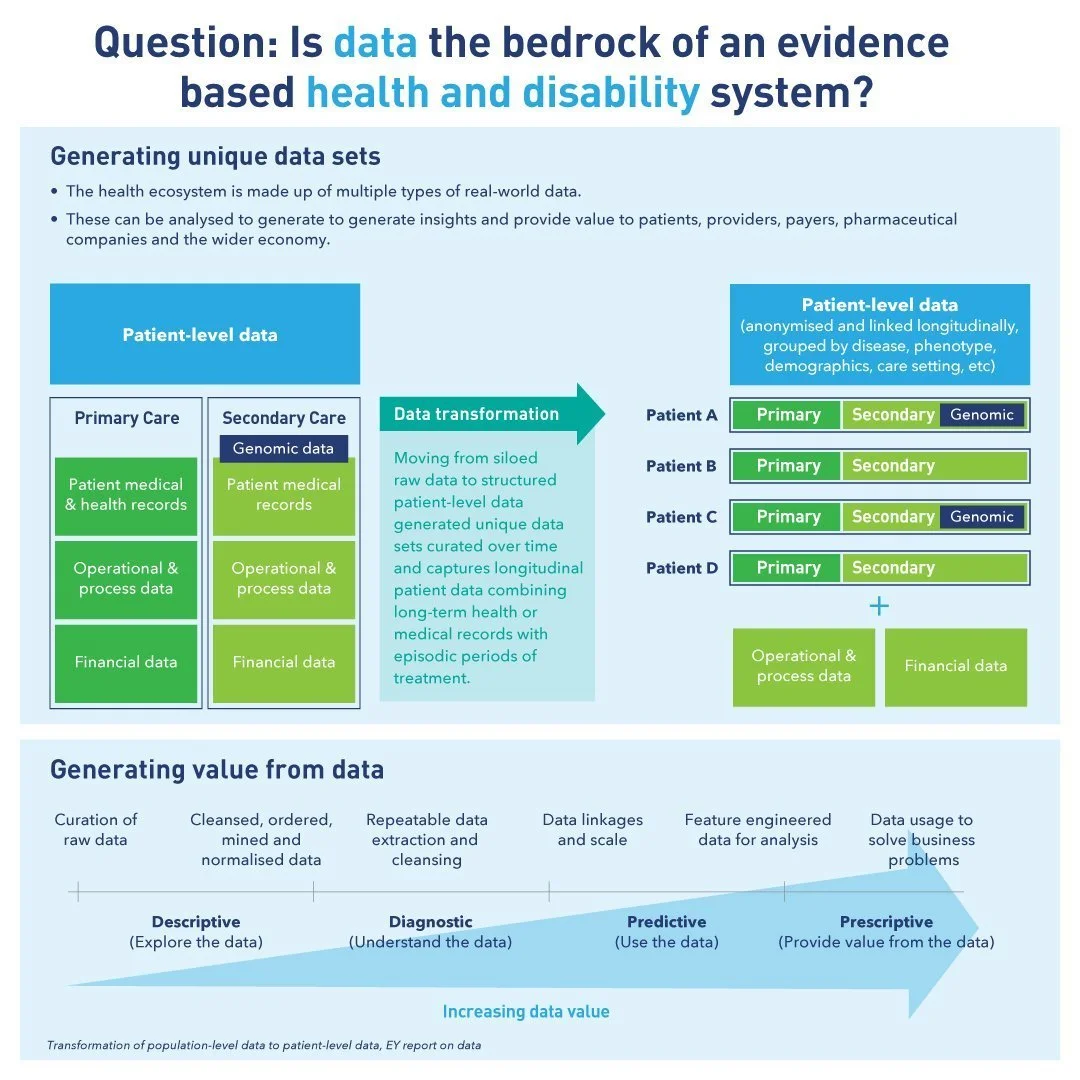
Is data the bedrock of an evidence bad health and disability system?
The mission of health care institutions demands effective and efficient medical data for evidence-based intervention. Installing an appropriate health care data management system with valid case definition enables efficient data extraction, improves communication for clinical decision making in medical practice, and clinical research, eventually upgrades the quality of health care services downstream.

Can community level cross-sector collaboration break healthcare barriers?
If the healthcare sector had a slogan, “we’re all in it together,” might be the leading contender ever since the COVID-19 pandemic emerged. Effective partnerships are essential for community-based solutions for advancing health equity. Many different stakeholders can lead or participate in implementing such solutions. Partners are able to deploy unique skills and resources to serve a variety of roles. The concepts of disruption, innovation, paradigm shift, and design thinking have become guiding principles for engagement in cross-sector work.

Become your own best advocate in the healthcare system
Self-advocacy means speaking up for yourself, making your own choices about your life, learning how to get information so that you can understand things that are interesting to you, finding out who will support you in your journey, and reaching out to others when you need help and friendship. It also involves knowing your rights and responsibilities, solving problems, listening, and learning, developing self-determination.

Does the statement “a built hospital bed is a filled hospital bed” still hold true?
Induced demand (ID) is a long debated topic in the field of health economics. It is defined as the change in demand for healthcare associated with the discretionary influence of providers over their patients. As a complex and multi-dimensional phenomenon, ID is a major challenge for health systems worldwide that creates an imbalance between needs and available resources, thus increasing the incidence of a health expenditure rise.

How will we achieve the ‘locality approach’ with our new health system?
For a while now, there has been a strong case to take a second look at the structure of NZ’s health system. Earlier this year, the government announced a major restructure of New Zealand’s health system. DHBs will be replaced by primary and community care organised in locality networks.

The only real mistake is the one from which we learn nothing
In healthcare, mistakes can have consequences that can vary from losing time to affecting patient outcomes. Without doubt, healthcare presents special challenges where judgment and individuality are involved.

Governance in healthcare series Part III - Startup Boards
Bad boards destroy more companies than bad management or bad tech. The business environment has changed enormously over the past decade. However, our level of business model innovation has not been matched in the way we operate our boards. There has been little innovation in board practice and it is demonstrably falling short of being fit-for-purpose.

Wicked problems - Healthcare
In 1973, Rittel and Webber introduced the term ‘wicked problem’ into social planning vocabulary. Wicked issues are different because traditional processes can’t resolve them. A wicked problem has innumerable causes, is tough to describe, and doesn’t have a right answer. Healthcare is a prime example.

Governance in healthcare series Part II: Corporate Governance
In the previous post, we briefly looked at clinical governance which includes caring for patients, managing clinical practices and administration. We now turn to corporate governance.

Governance in healthcare series Part I: Clinical Governance
Governance is a framework that accounts for all the processes of governing organisations and businesses. The role of governance in healthcare organisations looks a bit different than it does in other types of industries.

Gabe’s Aceso story with Morgo’s podcast series
Morgo's latest podcast is interviewing our CEO, Gabe Rijpma.
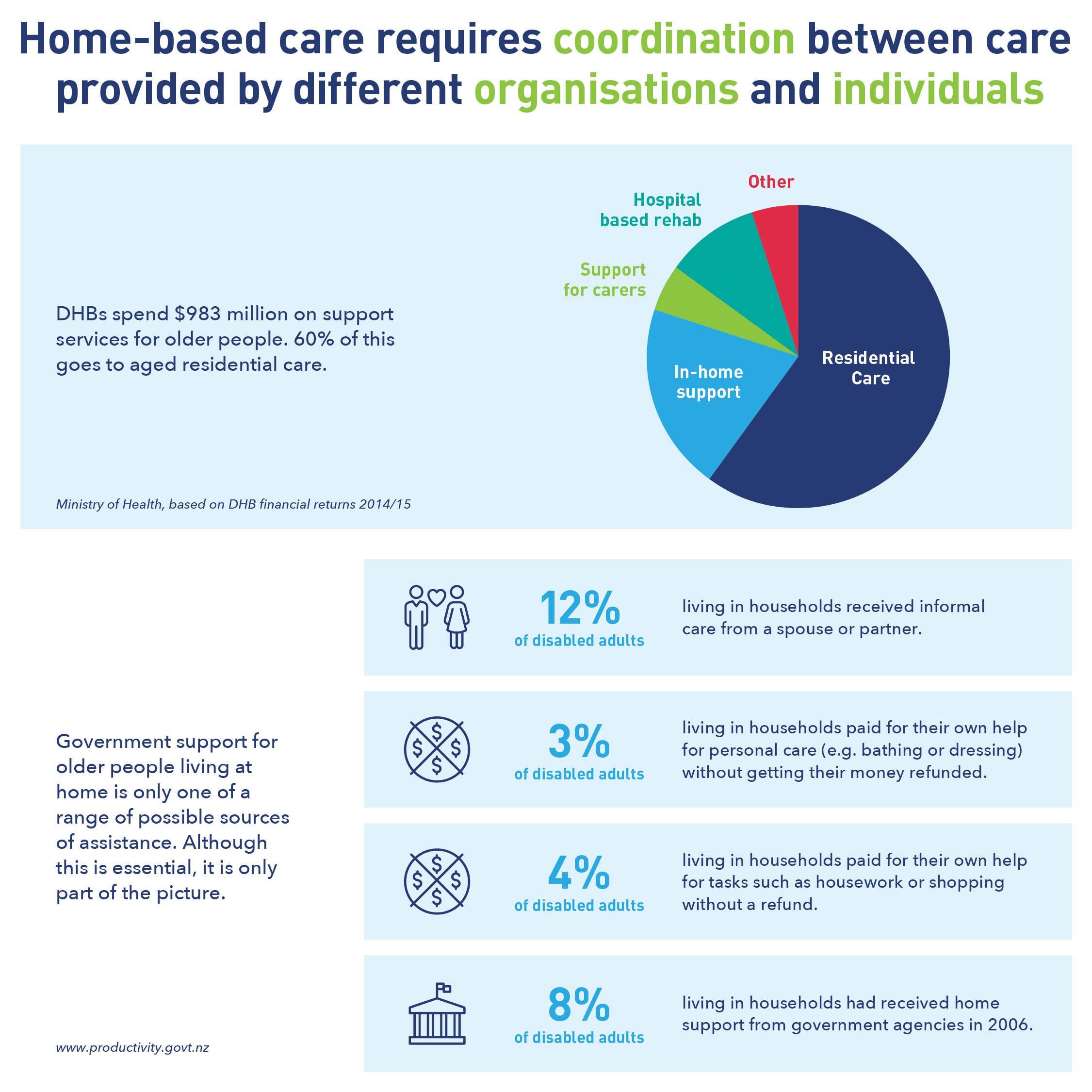
Home-based care: Coordination between care providers
Most people experience a decline in health and ability as they age. Just over half of New Zealanders aged 65-74 and nearly 2/3rds of those aged 75 years and over have two or more long-term conditions. Improving the health and wellbeing of older people through home-based support is not an easy outcome to achieve.

New Zealand’s Health System Indicators
Health targets were a set of national performance measures in place from 2007 to 2020, designed to improve the performance of health services. However, health targets have had their share of criticism of never being a reliable assessment of how well health services are performing. These targets have now been replaced by the Health System Indicators (HSI).

Digital therapeutics and the changing face of healthcare
Historically healthcare has been delivered offline. This is changing with the emergence of digital therapeutics (DTx). Worldwide, there are over 318,000 mobile health apps available, and around 200 apps are being added to app stores each day. To ensure patient and consumer safety, it is important that health apps are assessed for safety, functionality, quality, data protection, data security, and positive effects on care.

Balancing supply and demand in our health system
The Allied Health Science and Technical workforce encompass over 40 professions and more than 40,000 individual professionals. It represents the second largest health workforce in New Zealand.
How do we shift to a sustainable healthcare system?
International competition for doctors is increasing. Despite efforts in many OECD countries to become medically self-sufficient by training more doctors, significant shortages are forecast. Historically, New Zealand has been a net importer of the workforce.

Will our health system cope with more COVID-19 ICU patients?
According to data from worldwide outbreaks, around 5% of people who test positive for COVID-19 end up requiring intensive care. Intensive care services are fundamental to delivering healthcare.

Is the private health system complimentary or detrimental?
Equity and workforce shortages are important concerns under New Zealand's current health system. Adding to the conversation, is the question around whether the private health system is complementary or detrimental to the public system.

Lessening the burden on our healthcare system
Lessening the burden on our health system requires that we keep people well for longer, with care provided close to home.
